How do opticians test for glaucoma?
There are a variety of tests that you may undergo when you have an eye exam for glaucoma. Early detection of the condition is vital to ensure your vision is protected from the damage often caused by the condition. A complete glaucoma eye exam typically consists of up to six tests which are detailed below.

Tonometry
Tonometry measures the pressure inside the eye. Increased eye pressure is a serious risk factor for glaucoma and therefore important to monitor. The test itself is quick, easy and painless. The optometrist will use a medicated eye drop to numb the eye before a tiny instrument called a tonometer very gently touches the surface of the cornea (the clear window at the front of the eye) to measure the pressure of the eye. Pressure can also be measured with non-contact tonometry using a warm puff of air.
Pressure will be shown as a number followed by the abbreviation “mm Hg” (millimetres of mercury – a standard measure of pressure). The range for normal pressure is between 12mm and 22mm however, a higher than average result does not always mean you have glaucoma and some people have glaucoma at pressures lower than the average. It all depends on the unique individual and is an indicator only.
Pachymetry
Pachymetry measures the thickness of your cornea with a simple, painless test using a small probe called a pachymeter. After numbing your eyes with drops, the pachymeter will be gently placed on the eye to measure its thickness. This measurement can help your optometrist to better understand the results of the tonometry test because corneal thickness can often influence eye pressure. For example, a thin cornea may lead to misleadingly low eye pressure readings. It is also common for thin corneas to be a risk factor for glaucoma, so this test provides vital information for your optometrist to develop the right treatment plan.
Ophthalmoscopy
This procedure uses eye drops to dilate the pupil so that the optometrist can get a clearer view to inspect the optic nerve at the back of the eye. This is achieved by using an instrument called an ophthalmoscope to look directly through the pupil. The optometrist can then assess the optic nerve in more detail by magnifying it with a small lighting device. The shape and colour of the optic nerve can indicate whether or not there is glaucoma-related damage present in the eye and how extensive this damage is. If the optic nerve appears unusual or the pressure inside your eye is not considered to be in the normal range then you may be required to undergo further glaucoma exams: perimetry and gonioscopy.
Perimetry Or ‘Visual Field Test’
Perimetry is a test that evaluates your visual field to determine whether your vision has been affected by glaucoma. The test is not painful and only takes a few minutes for each eye. It usually involves looking straight ahead at a light whilst other lights appear in your peripherals. This helps to draw a map of the vision all around your field of view to see if any areas of your peripheral vision are being lost and the rate at which this is progressing. Your optometrist may want to repeat the test to ensure that the results are accurate before explaining how severe the disease is. After glaucoma has been diagnosed, visual field tests are usually carried out once or twice throughout the year to check for any changes to your vision.
Gonioscopy
Gonioscopy examines the angle where the iris (the coloured part of the eye) meets the cornea and where fluid drains from the eye. Your eyes will need to be numbed and dilated with medicated drops. A goniolens (a special hand-held contact lens with mirrors inside) is gently placed on the surface of the eye so that your optometrist can assess the inside of the eye from different directions. This helps to determine whether the angle is open or narrow. An open angle is a possible sign of chronic glaucoma whereas a narrow-angle may indicate acute glaucoma. The procedure is simple and painless.
Imaging Technology
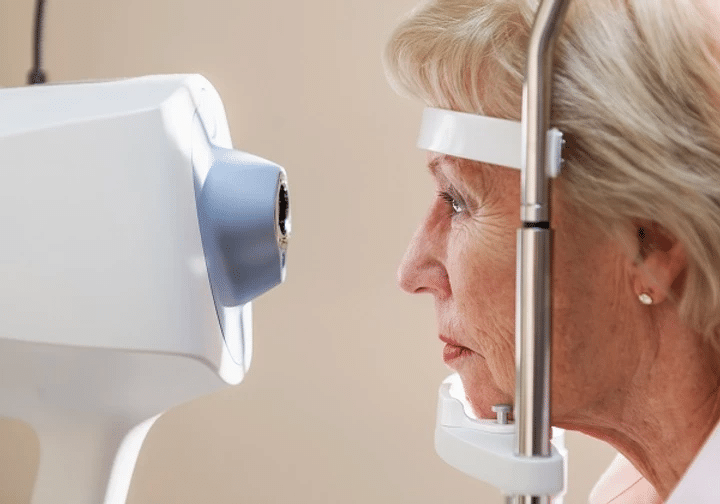
Glaucoma imaging tests can now be carried out using one of the new image analysis systems that are now available in the optical industry. They are a reliable method of monitoring the progression of glaucoma by providing highly sophisticated images of the retina using a digital camera or other technologies such as OCT to capture the details of the optic nerve. The tests are non-invasive and only require dilating drops. The results are available immediately and can be projected in front of you for discussion after your testing is complete.
Glaucoma can be quite difficult to diagnose and therefore it is vital to evaluate the optic nerve carefully to ensure the best treatment is provided. If your condition proves difficult to diagnose then you may be referred to a glaucoma specialist.
Patient story
At Book An Eye Test, we always like to share good new stories of our trusted local independent opticians.
A patient (Mark A Preston) of Wooding Opticians in Blackpool attended the practice for a routine eye examination as he was having headaches on the side of his head which he thought might relate to his eyesight.
After an advanced eye examination using the OCT machine, the optometrist discovered that the optic nerve that connects his eyes to his brain was damaged (otherwise known as glaucoma) and was referred to the specialist where he was treated stopping Mark from potentially going blind.
Related articles